The year 2025 marked a period of profound transformation and volatility for American public health, characterized by sweeping leadership changes, aggressive fiscal restructuring, and a fundamental shift in vaccine policy. Under the second Trump administration, the Department of Health and Human Services (HHS) underwent a radical ideological pivot that has sparked intense debate over the future of scientific integrity and healthcare accessibility.
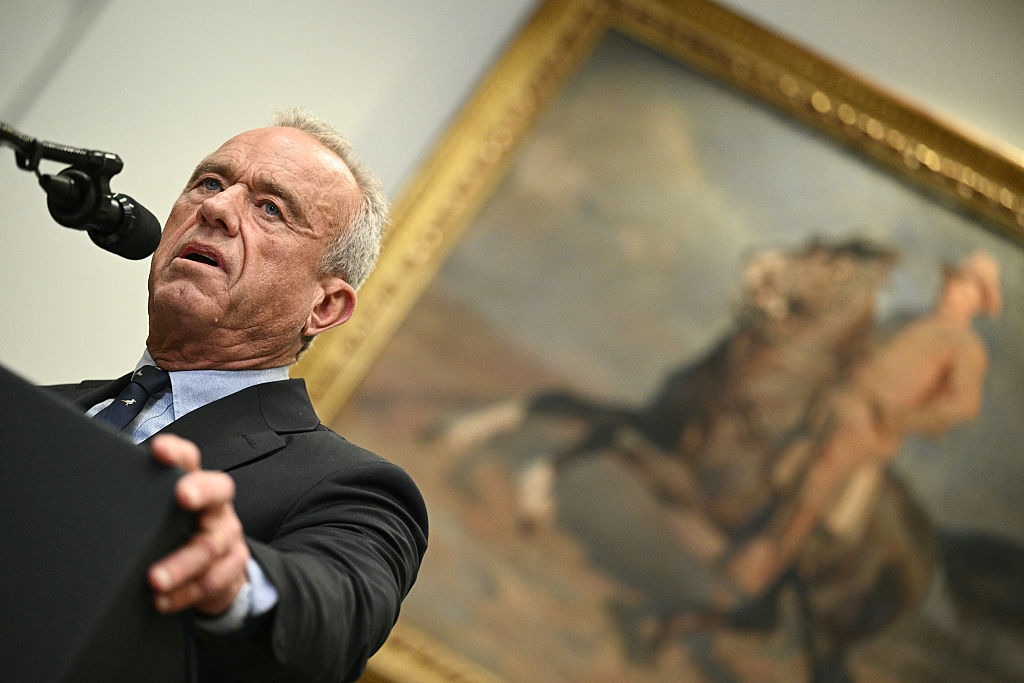
The Kennedy Appointment and Institutional Overhaul
In February 2025, Robert F. Kennedy Jr. was confirmed as HHS Secretary in a narrow 52-48 vote. Despite significant political resistance rooted in his history of vaccine skepticism, Kennedy immediately initiated a comprehensive restructuring of the agency. His actions included the mass cancellation of grants and the replacement of established scientists with figures known for questioning immunization standards.
The most prominent example of this shift occurred on June 9, when Kennedy dismissed all 17 members of the CDC’s Advisory Committee on Immunization Practices (ACIP). This body, traditionally composed of clinicians and public health leaders, was replaced by eight members who have echoed misinformation regarding COVID-19. This internal friction was further highlighted by the brief tenure of CDC Director Susan Monarez, who was ousted in August after only a month of confirmed service. Monarez later testified that her removal was a direct result of her efforts to maintain scientific integrity against Kennedy’s verbal attacks.
Fiscal Retrenchment and Insurance Stability
Legislative changes in 2025 have significantly altered the federal healthcare safety net. A major funding bill passed in the spring introduced $1.1 trillion in cuts to Medicaid and the Affordable Care Act (ACA) marketplaces by implementing stricter work and eligibility requirements. Projections suggest that 15 million people could lose coverage by 2034, with rural hospitals facing the greatest risk of destabilization. While Congress established a $50 billion rural health fund to mitigate these effects, experts contend this amount is insufficient to offset the projected losses.
Simultaneously, the expiration of enhanced ACA premium tax credits on December 31 threatens the coverage of another 22 million Americans. The political impasse over these subsidies led to a 43-day government shutdown, leaving the future of affordable insurance premiums in a state of deep uncertainty.
Altering the Medical Landscape
The administration’s “Make America Healthy Again” initiative led to the systematic revision of federal vaccination recommendations for several conditions, including influenza, RSV, and measles. These changes drew immediate condemnation from the American Medical Association (AMA) and the American Academy of Pediatrics, raising concerns about future insurance coverage for routine immunizations.
Beyond policy, the administration impacted the healthcare workforce by increasing H-1B visa application fees from $4,500 to $10,000. Given that international graduates comprise over 20% of practicing family doctors, the medical community warns that this fee hike will stifle the talent pipeline and exacerbate existing labor shortages in the healthcare sector.