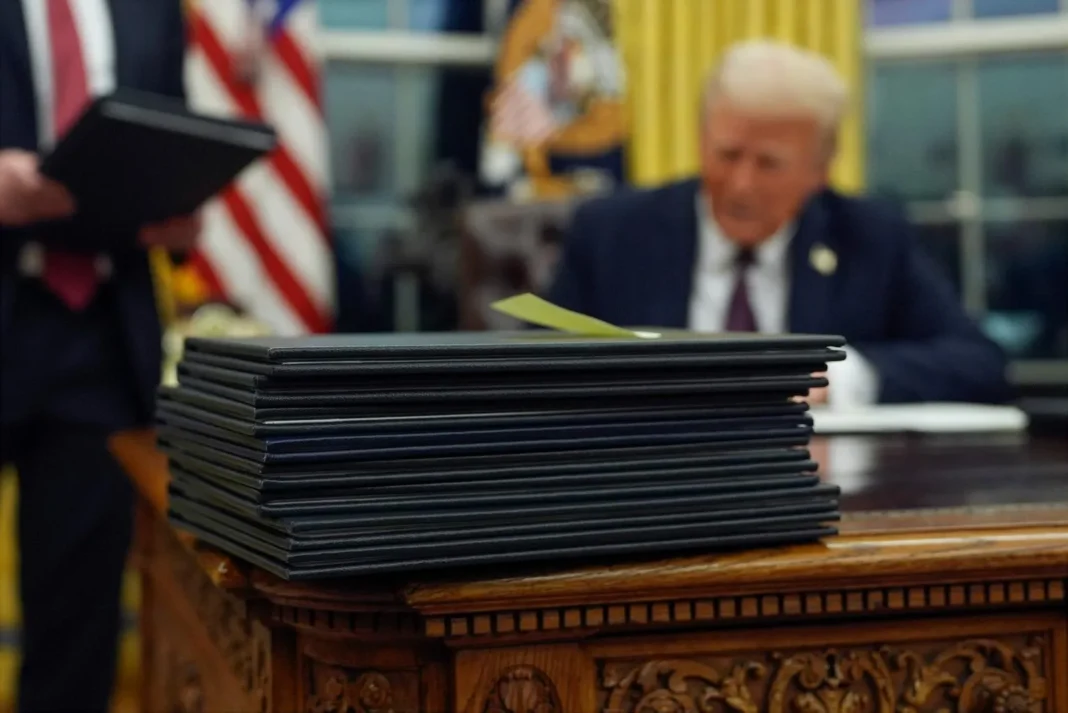
WASHINGTON — Tens of millions of Americans face a volatile healthcare landscape in 2026 as sweeping legislative changes from the Trump administration’s “big, beautiful bill” take effect. The most immediate impact involves the expiration of Affordable Care Act (ACA) premium tax credits, which is projected to leave 4.8 million more people uninsured and cause costs to “dramatically rise” for 22 million others.
Under the leadership of Health and Human Services Secretary Robert F. Kennedy Jr., the administration is also spearheading a comprehensive overhaul of public health policy. Key initiatives include a restructured federal vaccine advisory panel and a new pediatric immunization schedule that mirrors more conservative international models.
The Impact of the “Subsidy Cliff” and Legislative Shifts
The healthcare environment is undergoing a fundamental transformation as temporary pandemic-era protections yield to fiscal tightening and redirected federal priorities.
- Financial Reconciliation: Marketplace enrollees must now repay the full amount of any excess premium tax credits if their actual income exceeds their initial estimates. Previously, tax liability caps protected many from high repayment costs.
- Restricted Eligibility: New requirements limit premium credits to specific noncitizen groups, such as green-card holders and Cuban or Haitian entrants. Categories like refugees and asylum-seekers no longer qualify for this financial assistance.
- Medicaid Incentives: Federal incentives that encouraged states to expand Medicaid coverage are largely ending. While states with existing expansions retain their current funding levels, the window for new states to qualify for enhanced two-year bonuses closed on Jan. 1.
- Education Constraints: Aspiring physicians will face new financial hurdles as the government implements caps on Federal Direct Stafford and PLUS Loans beginning July 1, potentially impacting the future medical workforce.
A New Direction for Public Health
Beyond insurance and finance, the Department of Health and Human Services is actively revising core medical recommendations. The proposed pediatric vaccine schedule aims to reduce the number of recommended shots, citing a desire to align U.S. policy with countries like Denmark. The CDC’s vaccine advisory panel is scheduled to meet in February, June, and October to finalize these shifts, signaling a period of significant transition for American clinical practice.